- Patients who feel their preferences are respected and heard - that’s the idea behind patient-centred healthcare.
- Your pharmacy team works with you to develop care strategies that fit both your needs and your values.
- This type of care also taps into technology to make the experience easier for you.
What is patient-centred care, and how is your pharmacy team using it to help you manage your diabetes?
The Institute of Medicine explains that patient-centred care respects, and responds to, individual patient preferences and needs. As the patient, your values are meant to guide all clinical decisions. While you may not get exactly what you want all the time, your preferences will be carefully considered when your care team – which includes your pharmacist – provides patient-centred care.
This type of care involves four different parts.
1. Patient-centred care balances the professional knowledge of the care provider with the personal knowledge held by you and your family.
You and your family know your situation best. Your pharmacist brings years of education and practical experience in understanding how medications work. In patient-centred care, we combine this knowledge to tailor a strategy specific for you and your needs. Your pharmacist takes the time to understand your health goals, and gives you information on which medications may be best suited for you. Your care might also include recommendations on lifestyle adjustments, such as getting more physical activity or ways to improve nutrition.
2. Patient-centred care ensures that you are heard, valued, and engaged in conversations and decisions about your own healthcare.
Good communication is key to your relationship with any healthcare provider. The type of questions your pharmacist asks can help.
Closed-ended questions can be answered with yes or no. For example:
- Have you experienced any side effects from this medication?
- Do you have any questions?
- Do you ever forget to take your medication?
Sometimes a closed-ended question is necessary and appropriate. However, many people often automatically answer no to this type of question! The conversation ends, and it can feel awkward to ask anything else.
In contrast, open-ended questions encourage you to provide more detail about your experiences and personal situation. For example:
- What side effects have you noticed?
- What questions do you have?
- What might help you to remember to take your medication? Tell me how you remember to take your medication.
In asking an open-ended question, your pharmacist gathers more information to understand more about your specific condition, and your needs and goals.
Healthcare providers should also ask about what concerns you most at that moment. Your diabetes may not be at the top of the list if you have had a headache for several days or your arthritis is flaring up. Instead of focusing only on diabetes, your current concerns can also be addressed – a significant part of the patient-centred partnership.
3. Patient-centred care focuses on your goals as well as the expertise of the healthcare team.
You may be used to having healthcare providers identify goals for you, instead of the other way around. For instance, you may have been told to keep your blood glucose within a set range, or your A1c below a specific number. Research shows that certain goals offer the best chance of effectively managing diabetes and leading a healthy life, now and in the future. Healthcare providers are likely to recommend working toward those goals.
However, patient-centred care also takes your personal goals into account. Perhaps you want to have more energy. Maybe you need to manage your diabetes well with the pressures of a demanding job. You might want to include more activity so you can play with your children or grandchildren. Describe your goals to your pharmacist and other healthcare team members. Your team examines your goals with you, and structures your diabetes care in a way that allows you to achieve them.
Your pharmacist can work with you to help you achieve goals in ways that are meaningful for you. Let’s say that you have been told that you should be testing your blood glucose twice each day, but you only test once a week. If you share that information, your team can help design a more realistic plan. Perhaps you might agree to vary the time and day of week when you do that one test, or to gradually increase the number of tests you do each week. By working together to set goals that are both helpful and realistic, you can improve your health outcomes. You should be involved in setting goals that you understand, and feel confident you can reach them.
4. Patient-centred care adds knowledge from all team members.
Do you find yourself repeating the same details when dealing with the healthcare system? Even if you have visited the same pharmacy for years, you may have to deal with a new pharmacist on duty or a team member whom you have never met. It can feel frustrating to have to start over with someone who doesn’t know you.
Technology can help. The ability to document your health issues and the care you are receiving continues to improve. In many provinces, pharmacists can see and, in some cases, add to the information on your provincial health profile. This allows for better communication about your health among your care providers. It also helps each health care provider to focus on their area of expertise. Seeing the big picture of your health and the care you are receiving helps your pharmacist to ensure your medications are appropriate for your situation.
Community pharmacists can also work with you to develop a care plan specific for you, and to review the medications you are taking. Often, this involves making an appointment to have a one-on-one discussion with the pharmacist about your diabetes goals. The pharmacist will gather information about your health, including your diabetes management. Each medication will be assessed to ensure you are getting the greatest benefit. How are you taking your medications? When are you taking them? Do you know why you are taking them? With this information, the pharmacist can decide whether adjustments are needed. Perhaps several medications could be combined in one, or a new medication might be more effective. Your pharmacist may also ask about adult immunizations and what you are doing to prevent getting sick. For instance, you may be due for a flu shot or need your tetanus vaccination updated.
When details like these are documented in your plan, the next care provider can clearly see your goals. They can also see where your plan left off, and where to begin work with you on the next steps. In some provinces, pharmacists may be able to initiate medication changes to better improve your health. Speak to your own pharmacist and learn about the professional services available to you.
A key outcome in centring care around patients is helping more people to meet their treatment plans. Even with all the advances in diabetes care over the past decade, there is still a lot of opportunity to improve the health of Canadians living with diabetes. Part of this challenge involves what is called adherence. The World Health Organization defines adherence as “the degree to which the person’s behaviour corresponds with the agreed recommendations from a healthcare provider.”
The word ‘agreed’ is key. In patient-centred care, you and your healthcare team should agree on what you need to do to manage your diabetes effectively. Agreeing to take your metformin three times per day but only taking it once per day is an example of non-adherence. At one time, your pharmacist might have simply told or reminded you to take the tablets three times each day. A patient-centred approach involves finding out why it is difficult for you to take your metformin regularly. Perhaps the medication is costly, or you find the tablets hard to swallow. Maybe you forget to take your tablets, or you don’t take them because of side effects that worry you. With this information, your pharmacist can work with you to provide strategies that fit into your overall life goals. More support may help you to take your metformin regularly. No matter what your goal is, patient-centred care works the same way – from how often you check your blood glucose or A1c to how much physical activity you get and how often you choose nutritious foods. Research shows that meeting your diabetes care goals improves your health and lowers your chances of experiencing complications.
Your community pharmacist has always been an accessible, knowledgeable partner in your healthcare. Adding in patient-centred care strategies allows us to support you more fully. If you have questions about patient-centred care, or wish to develop your own personalised care plan, your pharmacist is on hand to help.
WRITTEN BY: Stacy Johnson, BSc (Pharm), MBA, Director of Pharmacy Programs & Professional Development in Calgary, AB.
Key points:
- Diabetes can be challenging! It’s normal to find yourself feeling angry, sad or frustrated.
- Diabetes distress is real. Diabetes Canada uses this term to describe the difficult emotions that accompany living with diabetes.
- Protecting your mental health is a key part of managing diabetes well.
Each day, we experience a wide range of emotions, from highs to lows – joy, sadness, excitement, anger, pride and anxiety. If you are living with a chronic health condition like diabetes, it’s normal to feel difficult emotions. Still, looking on the bright side can help to protect your mental health.
Learning that you have diabetes can often bring feelings of anger, sadness and denial. As time passes, frustration or continuing anger can deepen into depression. Being diagnosed with diabetes can change the way you feel about yourself. People often have a new vision of themselves as ‘sick’ or ‘not quite well.’ It is tempting to use denial as a way of dealing with this changed body image. You may feel that if you just eat and do as you want, no one will ever know about the disease. You can pretend nothing has changed.
However, denial is both physically and mentally dangerous. Uncontrolled diabetes (high glucose levels) makes depression worse. A struggle with depression may keep you from even trying to learn more about your diabetes, an essential part of managing this condition. Depression makes it harder than ever to eat well and get enough physical activity. It is common to feel that life is over, and not even try to manage your diabetes.
Even if you are managing your diabetes well, it’s easy to fall prey to depression and negative feelings. Both types of diabetes get more difficult to manage as time goes on. In Type I diabetes, the number of working beta cells (cells that make insulin) continues to decline. Once they are nearly all gone, blood glucose levels tend to swing even with regular food intake, exercise, and insulin doses. As glucose levels become more difficult to predict, you may feel very frustrated and frightened.
Type 2 diabetes is also progressive. It doesn’t just seem to get harder to manage – it really does get harder. As time passes, more medication and often insulin may be needed to manage the diabetes. Even if you have come to terms with your diabetes, eat well and exercise daily, this progression in itself can be depressing.

Difficult feelings and depression can often come from the way others respond to your condition. Imagine – you have waited all day to enjoy a carefully measured treat. It is not pleasant to be told, “You have diabetes – you can’t eat that!” It’s just as bad to have someone force a treat that you know you shouldn’t eat, saying, “I made this especially for you, surely one little piece won’t hurt.” Or to overhear, “I would love to have them over, but I don’t know what to give them to eat.” Some comments are rude, insensitive, and unthinking. Others are said in ignorance. Helping your friends and family learn that people with diabetes can eat a wide variety of foods can be empowering for you and make your life – and theirs – more fun!
The fear of being excluded can also make you feel helpless and depressed. Though you want to be included, the fear of changing glucose levels is very real. If the level is too low (hypoglycemia), you may stumble, have embarrassing mood swings or, more seriously, go unconscious. Such symptoms can put you and possibly others at risk. If the level is too high, it is difficult to concentrate. You may be very thirsty and need to go to the washroom very often. Social events can become more difficult. You may begin to refuse social outings, and to narrow your circle of friends.
If your diabetes stays out of control with high readings, it can lead to long-term complications. These include blindness, kidney disease, nerve disease, amputation and early heart disease. All of these conditions can make you feel different from everyone else.
Fighting negative feelings and overcoming depression is hard work in itself. If you are also dealing with the daily and unceasing demands of diabetes, it becomes even harder. No matter what you do, some days are difficult. You may need a lot of hope and emotional energy just to keep going. For some people with diabetes, life can be a constant battle for control.
Diabetes Canada defines diabetes distress as the negative emotions and burden of self-management related to living with diabetes. The term describes the difficult emotions that accompany a diabetes diagnosis. This includes the need to continually monitor your diabetes and treatment, ongoing worries about complications, and the potential changes to your personal and professional relationships.
HELPFUL WEBSITES
How can you protect your mental health?
One way to get through is to expect tough times and have a plan. Use ways of coping that have worked for you in the past. For instance, you might play or listen to music, go to the theatre or a movie with friends, or take a walk in the park when you are feeling stressed. Make a list of favourite things that make you feel happy. Refer to this list when you are feeling down.
Try exploring how diabetes fits into your life. Make a list of all the roles you play. These could include parent, child, grandparent, friend, volunteer, colleague, boss, employee, and client. Now list all the skills that you have, such as typist, teacher, musician, athlete, team player, reader, knitter, cook, and gardener. List your physical features: eye and hair colour, tall, short, thin, overweight, high blood pressure, hammer toes … diabetes. Of all the things you are, having diabetes is only a small piece. Though diabetes is part of the list, it is not the whole list.
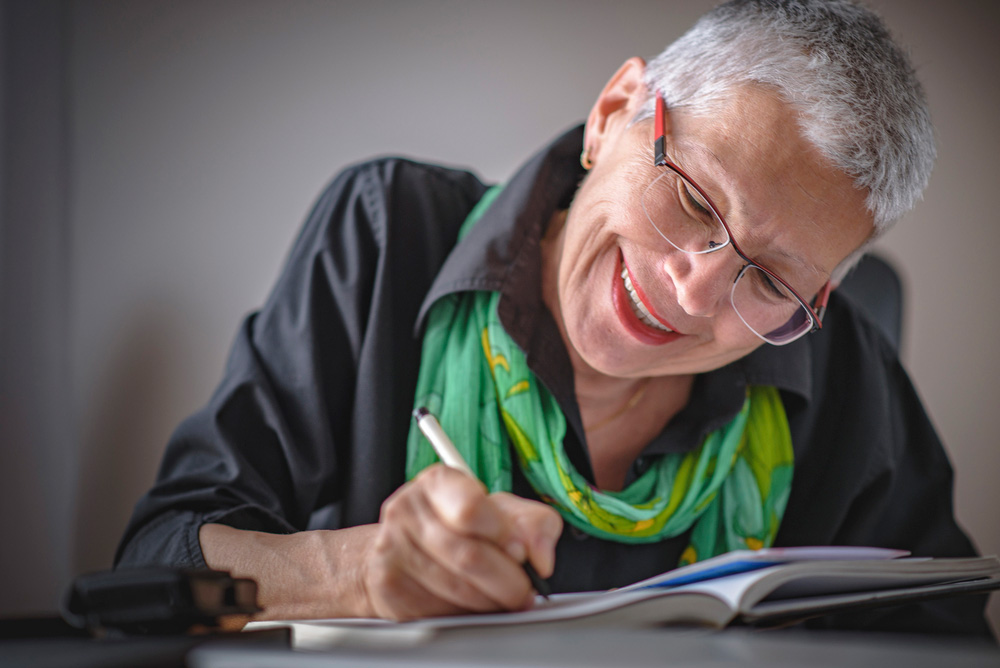
Spend time each day listing the positive things in your life. One idea (borrowed from Oprah!) is to keep a gratitude journal. List a few things each day that you are thankful for, such as a loving spouse, a cuddly pet, or a beautiful afternoon. Reread your lists to remind yourself of everything good in your life. Move your attention away from problems and errors.
Although they won’t go away, you have shifted gears. This is the ‘power of the positive.’ It can take some practice if you have allowed the negative to take over.
Another important strategy includes incorporating regular physical activity to benefit your mental health. This could be a walk with a friend, enjoying gardening or other yardwork, or participating in a team activity. (If you have been inactive for some time, talk to your doctor before starting any exercise program that is more strenuous than brisk walking.)
Other alternatives include employing a mindfulness practice or learning specific physical or mental relaxation strategies. There are many resources to help you get started. Ask your diabetes health care professional to help you determine your personal goals in order to develop a plan.
Some negative things, however, will always need sorting out. Do you find it easier to solve a problem if you discuss all the aspects with others? Or do you like to put all the good things about a plan in one column and all the bad things in another? There are many ways to help rehearse possible results. The key to good problem solving is thinking ahead to all good and bad possibilities.
If you need to talk things out, do you have a network of well-informed people? Do you value their input? Having social support has a very positive impact on overall health. Going over the same ground again and again can be difficult and lead to burnout. Consider saving your friends for fun, and use a diabetes health professional or a diabetes support group to discuss issues and concerns. This can also help your loved ones.
Family is important. Your family members are closest and most involved with your life and diabetes. However, they also have their own emotional responses to your diabetes. While some responses are helpful and supportive, others can make it harder for the person with diabetes. The relationship may need to change. For instance, parents feel concern and grief for their child who has diabetes. They may feel guilty and helpless. They worry and struggle with finding the limits of supervision and independence. All of the extra work and planning and balancing can leave parents feeling very overwhelmed. They may become angry with each other, the child with diabetes or other children in the family.
Brothers and sisters worry that they will also get diabetes. Sometimes they are so relieved it is not them that they feel guilty. If food and activities change for the entire family, other children may feel angry with the one with diabetes.
Learning about diabetes as a family is one way to work through negative responses. With time and support, children and families usually find a way to help each other. Favourite food choices may change or be spaced out, but they can usually be included. Since food for managing diabetes is healthy, everyone can eat the same way. It’s easier when everybody is involved in learning how to develop healthy eating habits.
For adults, a partner may be the one who is most involved. Finding the balance between supporting food choices that are healthy and acting like the ‘food police’ is a challenge. Nagging or know-it all attitudes are not very helpful. Though learning about diabetes together is useful, remember who it is that has the disease. One partner may be more involved in food purchasing and preparation, but both should know what will be on the shopping list and then the table.
Remember that every added problem or change in managing diabetes is difficult. It can be like being newly diagnosed again. The partnership may be stressed too. Some might view it as their own failure to keep on track. A partner who has tried to choose appropriate food and has supported and participated in the daily exercise program may feel the same sense of failure – “If only I had been more careful and encouraging.” While it is OK to feel this way, remember that failure may just be a change in the body’s ability to function efficiently and may not reflect anyone’s management choices. We cannot slow time and aging.
Finally, find the diabetes educators in your community. These experts can work with you and your family to help you get through rough spots. They may be nurses, dietitians, pharmacists, social workers, or doctors.
Keep in mind that it is normal to experience feelings of grief, denial, and sadness when dealing with diabetes in your family. If these feelings persist and interfere with your usual sleep, eating and social patterns, see your doctor. Clinical depression and anxiety are more common in people with diabetes, and other therapies such as medication may be required. As with all health issues, your mental health can change over time. Make sure that you are discussing your mental health with your diabetes health care professional on a regular basis. By asking certain questions, they can quickly assess how your mental health is at that moment and provide specific recommendations for treatments.
Remember, your family and friends love you and usually want to be supportive in whatever way is best for you.
WRITTEN BY: Susan Roe-Finlay, RN, MSc, CDE.
EDITED BY: Stacy Johnson, BSc (Pharm), MBA

- Wondering what heart-healthy lifestyle changes to make after a diabetes diagnosis? Relax! You just need to put the same health advice you’ve already heard into action.
- The top tips for better health are those you’ve always heard - quitting smoking, lowering your stress levels, exercising regularly and eating a heart-healthy diet.
- Research shows that when it comes to protecting heart health, the simple and delicious Mediterranean Diet is even better than a low-fat diet.
Nearly 11.7 million Canadians live with diabetes or prediabetes. If you’re one of them, you already know how this condition could affect your health. Over time, uncontrolled blood glucose levels can damage various organs, blood vessels and nerves. Diabetes also puts you at a higher risk of developing heart disease and stroke. Fortunately, you can take action to protect your body and your heart.
How does diabetes affect my health?
Having diabetes means that your body is not able to balance blood glucose levels. Depending on the type of diabetes, the body is unable to make insulin, use insulin, or both. Insulin deficiency means that your pancreas has lowered the amount of insulin it makes. If your body cannot use insulin as well as it should, this is called insulin resistance.
A diabetes diagnosis can be startling. You may feel that you should be making sweeping changes. If you’re overwhelmed, relax. You can actively prevent complications by following the same health advice you’ve always heard.
- Quit smoking.
- Lower your stress levels.
- Exercise regularly.
- Follow a heart-healthy diet.
When you understand what is most important, you can make better decisions from moment to moment. Choices that you can stick with confidently are best.
Recommendations from the Heart and Stroke Foundation of Canada
- Healthier choices help reduce many of the risk factors for heart disease and stroke.
- Eat well. Focus on vegetables and fruit, whole grain foods, and variety in your protein choices. Limit ultra-processed foods, sugar, salt and fats.
- Get moving and stay active.
- Maintain a healthy weight. Where you carry your weight is also important. Aim for a healthy waist size.
- Stop smoking. (Your pharmacy may have a program for helping people quit.) Avoid second-hand smoke as well.
- Manage your stress. Understand what makes you feel stressed, and learn effective ways to respond to it.
- Speak with your diabetes care team, and check out the Heart and Stroke Healthy Living webpage to learn more:
Diabetes health targets
Your diabetes care team can advise you on assessing and managing your diabetes to keep:
- blood glucose levels within target range
- A1c at 7.0% or less
- blood pressure below 130/80 mmHg
- LDL (harmful) cholesterol below 2.0 mmol/L.
What are some heart-healthy food choices?
One of the most well-known heart healthy diets is called the Mediterranean Diet. Research shows that compared to a low-fat diet, it can help lower the rate of heart attack, stroke, and even death from heart-related causes.
A Mediterranean-style diet focuses on eating plant-based foods. It gives you fibre, phytochemicals, vitamins, minerals, lean protein and mono-unsaturated fat. It is also lower in saturated fat, sodium and added sugar. Basically, this diet gives you more of the good stuff your body needs. Even better, it suggests eating super-tasty and colourful foods that are sure to keep your taste buds happy.
After just a few changes, you can begin to benefit from the Mediterranean Diet. Once those habits feel comfortable, stick with and slowly build on them. Remember, your current eating habits did not develop overnight. You shouldn’t expect to change them overnight either.
One advantage of the Mediterranean diet is that it helps to raise “good” (HDL) levels of fat while countering the “lousy” (LDL) types. Triglycerides - a lipid or fat that provides energy – are a stickier form of cholesterol that can cause issues with the heart, even when levels are in normal range. Higher triglyceride levels are common among people who have diabetes. Along with better fats, the fibre-rich foods and whole grains in the Mediterranean diet can lower LDL cholesterol levels. For those who find it difficult to keep LDL consistently below 2.0 mmol/L, statin medications may be a good option.
What are the top tips from the Mediterranean Diet?
- Eat fruits and vegetables, beans and legumes, nuts and seeds, cereals and whole grains every day.
- Use olive oil as your main source of added fat in your cooking.
- Eat fish and poultry a few times a week.
- Limit how often you eat sweets, desserts and dairy products, as well as red and processed meats.
- Wine with meals is often associated with the Mediterranean diet. If wine is appealing, consume it in moderation. For wine, one standard drink is 142 mL (5 ounces). Alcohol may be associated with other health risks, so if you do not drink wine already, it is not recommended that you do so now. Speak with your doctor to find out if alcohol is safe for you. Also, remember that water is important for hydration.
Snack and meal inspiration
- Start your day on the right foot. Make a bowl of oatmeal porridge cooked with unsweetened non-dairy milk, berries and crushed walnuts.
- Not a fan of oatmeal? No problem! Instead, opt for a mixed-vegetable omelette with a side of whole grain toast and sliced avocado for breakfast.
- If you feel tuckered out by mid-morning, grab some plain Greek yogurt with a handful of blueberries to re-energize you before lunch.
- Make your lunch count! Enjoy a mixed green salad with olive oil and balsamic vinaigrette, roasted pumpkin seeds and a salmon salad sandwich for an extra heart-healthy kick.
- Let’s not forget the mighty bean. Prepare a mixed bean salad with an array of your favourite vegetables as a fibre-packed, meatless lunch choice.
- Curb that hunger. Snack on a handful of almonds before dinner to prevent your hunger from taking charge.
- Feast your eyes (and belly!). Enjoy a marinated baked chicken breast along with a side of roasted sweet potato, and plenty of bell peppers and zucchini to fill the rest of your plate.
- Craving something sweet? Apple slices with all-natural peanut butter make a refreshing nighttime snack when you feel hungry. Read labels carefully to avoid added sugar and sodium in some peanut butters.
Exercise is essential
It will come as no surprise to hear that physical activity is also crucial to safeguarding your health.
- Studies show people who exercise have improvements in A1c, triglyceride and cholesterol levels. They also have better cardiac and overall health compared to people who are less active.
- Check with your health care provider before starting any high intensity or competitive exercise. This is especially important if you are an older adult with current or previous vision, mobility, or heart issues.
- Try to do around 20 minutes of moderate to vigorous (sweat-inducing) activity each day. Remember that it’s most important to add some activity, even if it’s not for very long when you first begin. Ideally, you would be active for 150 minutes over the course of a week, with no more than two days off in a row.
- Resistance (weight) training is recommended along with aerobic exercise. Most studies done on this type of training suggest progressing to three sets of eight repetitions, at moderate to high intensity, three times a week or more.
- Remember that long periods of aerobic exercise may increase insulin sensitivity for up to two days. Monitor your blood glucose after aerobic exercise. If you use insulin, you may need to talk to your health care team about adjusting the amount.
- Avoid sitting for long periods of time. If you must sit when you work, make a habit of getting up and moving around from time to time. Being a couch potato is not good for your health.
Make the most of your team
Health care professionals can help you to manage your diabetes. If you haven’t seen your family doctor for a diabetes check-up recently, making an appointment is a good place to start. You will likely want to be seen every three to six months to check your HbA1c. (Some pharmacies now do HbA1c testing too.)
A registered dietitian specializes in food and nutrition. This health care professional can help you make sense of nutrition information and advise you about your diet. Ask your doctor for a referral to a local dietitian who specializes in diabetes care. Your community pharmacist, another key member of your health care team, can explain how certain medications can help manage your diabetes and protect your heart.
Although a diabetes diagnosis can feel overwhelming, you can take action to care for your health. Talk to your health care team about ways to protect your heart.
For cooking and nutrition inspiration:
Cookspiration, Dietitians of Canada: cookspiration.com
Diabetes Canada: diabetes.ca/managing-my-diabetes/recipes
Heart and Stroke Foundation: heartandstroke.ca/get-healthy/recipes
WRITTEN BY: Sanja Petrovic, RD, CDE, MSc.
REVIEWED AND UPDATED BY: Eric Hsu, RPh, CDE, a pharmacist in Vancouver, B.C.
Managing Diabetes Highlights:
- The food label lets you know if the food choice is right for you.
- Ingredients are listed from most to least, so make sure the first ones are what you actually want.
- Look at the serving size to see if it’s the amount you would normally eat.
- The % Daily Value shows how much of a certain nutrient is in a serving size. This tells you if there is a little or a lot of a nutrient in a serving size. 5% or less is a little and 15% or more is a lot.
- While the label may say a food is fat-free or no sugar added, sometimes that only applies to one nutrient. Check the ingredient list and other nutrients on the Nutrition Facts Table (NFT) to see if the food is the right choice for you.
Do you ever feel overwhelmed when trying to make healthy choices at the grocery store? With so many products on the shelves and more being added all the time, it is easy to be confused. The good news is that reading food labels can help you make the best food choices for you and your family as you navigate the aisles. The nutrition information on the labels of cans, packaged goods and frozen items is your guide to making healthy food choices. To develop your label-reading skills and understand what is included, take a closer look.
Start with the ingredient list
When reading a label, begin with the ingredient list. This list is required by law on all packaged foods. Ingredients are listed from most to least, so be sure that the first few ingredients are ones you want to be eating!
The Nutrition Facts table
Next, take a look at the Nutrition Facts table, which lists calories and 13 core nutrients. You will find that the table looks the same on different packages. This is an excellent source of information when you want to know more about the product. Start with the serving size, which will state an amount like six crackers or one tbsp or 250 mL. All nutrients are based on this amount. Be careful – the serving size may be more or less than the amount of food you would normally eat.
Also on the Nutrition Facts table is the % Daily Value (% DV). This tool is a benchmark for evaluating nutrient content quickly and easily. It is very helpful when comparing products and for making healthy choices. Nutrients are placed on a scale of zero to 100 percent. The higher the percentage, the more of that nutrient is present, so 5% DV or less means a little, while 15% DV or more means a lot. If the nutrient is one you want to eat more of, such as fibre, look for 15% DV or more. If it is a nutrient you would like to cut back on, such as sodium, look for 5% or less.

Package claims on food labels
Last but not least, consider the nutrient content claims on products. You might see statements like "no sugar added," "fat free," or "light." Buyer beware! Remember, the claim only focuses on one nutrient. By reading the ingredient list and Nutrition Facts table, you can get the whole picture and decide whether the product is cart-worthy.
If you have more questions on label reading, just ask. Dietitians are label-reading experts who can help navigate the grocery aisles and choose the best for you . Many dietitians are offering their services virtually. You can also get advice in planning grocery orders in advance. While reading labels does take a little longer, the benefits to your health are well worth the time.
Health Canada is improving food labels. A front-of-package nutrition symbol is required on foods that are high in one or more of these nutrients:
- sodium
- sugars
- saturated fat
The food industry has been given until January 1, 2026 to make this change.
However, you may start seeing the front-of-package nutrition symbol earlier.
For more information visit tinyurl.com/2s692z6n
WRITTEN BY: Laurie Barker Jackman, RD, a registered dietitian in Halifax, Nova Scotia.